Bursitis types: This is a condition that affects the bursae, which are the small, fluid-filled sacs that provide cushion for the:
- Muscles
- Tendons
- Bones near joints
The bursae make it easier for tissues to slide over each other. The body has around one hundred and sixty bursae. However, only a few become clinically affected. These include the:
- Wrist
- Elbow
- Shoulder
- Hips
- Knees
- The base of the big toe and heel
The condition typically presents near joints constantly being used repetitively, like a job, sports, house/yard chores, etc. What happens is one or more of the bursae sacs become inflamed, resulting in pain.
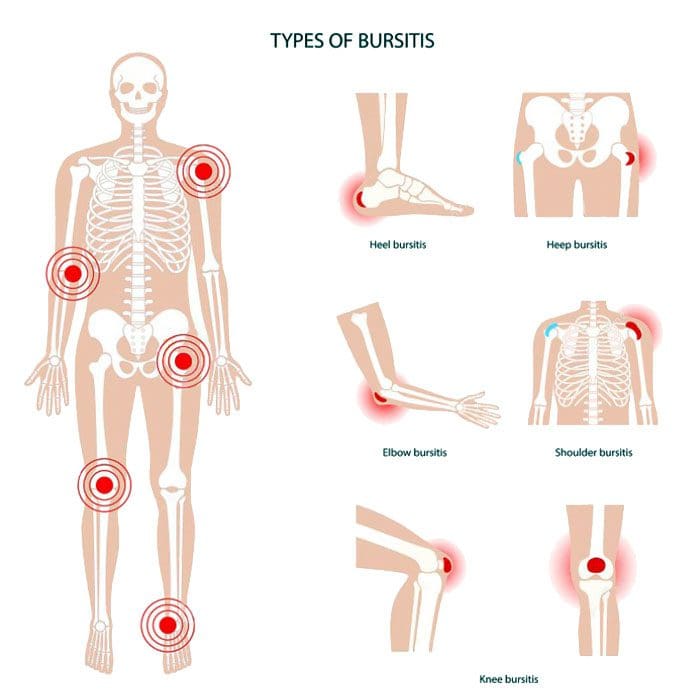
Table of Contents
Causes
- Inflamed or irritated bursae typically cause it from overuse or intense/vigorous activity.
- It can also be caused by bacterial infection.
- Arthritis and gout can also cause bursitis.
- Another cause is age.
- As tendons age, they can tear easily, lose their elasticity, and can’t take too much stress.
Intense physical activities can lead to bursitis. These include:
- Gardening
- Typing
- Working with a computer mouse
- Throwing
- Golf
- Tennis
- Manual tasks
- Carpentry
These types of activities can lead to incorrect posture, overuse, and injury/damage.
Symptoms
The main symptom is pain in and around the affected area that worsens with movement. Depending on the severity of the strain and the length of time it has been going on, the pain can be intense with active and passive movements. Other symptoms include:
- Tenderness
- Stiffness
- For some individuals, it can present as acute, with the intensity increasing.
- This happens when movement aggravates the condition.
Bursitis Types
Four major types include:
- Prepatellar
- Trochanteric
- Olecranon
- Retrocalcaneal
Prepatellar Bursitis
Prepatellar is an inflammation of the sac situated between the skin and the patella/kneecap. The most common causes are trauma from a fall and direct pressure/friction from repetitive kneeling. This is one of the bursitis types that can get infected. Overproduction of liquid places pressure on the other areas of the knee, causing swelling. Most individuals report swelling and knee pain just over the front of the knee.
Trochanteric Bursitis
This bursitis type goes over the lateral area of the hip. There is a distinctive tenderness and aching pain. This type is more common for individuals with arthritis conditions and fibromyalgia. This condition is also seen after surgery, mainly osteotomies. The bursa can become inflamed in case of injury or overuse. It tends to affect middle-aged or older folks. Common causes include:
- Muscle tears
- Hip injuries
- Tight hip or leg muscles
- Disc disease of the low back
- Leg-length inequality
- Improper walking technique from a minor injury or strain
- Overuse of the gluteal muscles
- Flat feet
- Improper footwear
Olecranon Bursitis
Olecranon is a common bursitis type. It is diagnosed by the appearance of swelling over the elbow. The swelling happens just behind the olecranon process of the ulna. The bursa can become infected. This bursitis does cause blood to rupture out, and fluid could be present. Individuals are advised to avoid leaning or resting on the elbows.
Retrocalcaneal Bursitis
This is characterized by pain in the Achilles tendon. Chronic inflammation of the bursa is brought on by friction, supination, and overpronation. The flexibility of the calf muscles can be significantly reduced. Severe pain and swelling of the posterior soft tissue in front of the Achilles tendon are common symptoms. This bursitis type is often accompanied by mid-portion insertional tendinosis.
Risk Of Getting Bursitis
Anybody at any age can develop bursitis, but older individuals, specifically those in their forties and beyond, are more susceptible. This comes from all the wear and tear of the muscles and bones.
Risk Factors
- Overpronation of the foot
- Leg length deviation
- Osteoarthritis
- Obesity
- Tight hamstring muscles
- Incorrect physical training
- Not stretching properly
Body Composition
When Inflammation Becomes Permanent
When white blood cells cause inflammation, it’s signaling that the body’s immune system works properly. The process works like this:
- Inflammation activates
- White blood cells attack the foreign invader
- The invader is neutralized
- The inflammation deactivates
This is how the body’s defense system naturally works. But, white blood cells are not the only type of cell that emit cytokines. Adipocytes or fat cells are another type of cell that can emit cytokines and cause inflammation. Scientists have learned that fat is an active endocrine organ that secretes various proteins and chemicals, including inflammatory cytokines. The body stores excess calories as fat to be used later for energy. When the body keeps adding more adipose tissue, cytokines are released by the fat cells, triggering inflammation. Obesity is characterized as a state of low-grade, chronic inflammation. Increased fat cells place the body in a constant state of stress activating immune responses. This means the body is in a constant state of inflammation with the immune system switch permanently on.
References
Aaron, Daniel L et al. “Four common types of bursitis: diagnosis and management.” The Journal of the American Academy of Orthopaedic Surgeons vol. 19,6 (2011): 359-67. doi:10.5435/00124635-201106000-00006
Coelho, Marisa et al. “Biochemistry of adipose tissue: an endocrine organ.” Archives of medical science: AMS vol. 9,2 (2013): 191-200. doi:10.5114/aoms.2013.33181
Khodaee, Morteza. “Common Superficial Bursitis.” American family physician vol. 95,4 (2017): 224-231.
Professional Scope of Practice *
The information herein on "Bursitis Types" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on this site and our family practice-based chiromed.com site, focusing on restoring health naturally for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Licensed as a Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multistate
Multistate Compact RN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card














